Latest News: News
Amanuiel Taddese

Email: yushy.zhou@student.unimelb.edu.au
- Orthopaedic research
- Arthroplasty
- Machine learning
- Health economics
- The University of Melbourne
- The University of Auckland
- St. Vincent’s Hospital Melbourne
Yushy Zhou
MBChB, PGDipSurgAnat (Distinc)
Yushy is a PhD candidate at OPUS focusing his research on how to improve patient selection in total knee joint replacement. This will involve the development of a decision support tool used to predict patient satisfaction and outcomes after surgery. The tool will use machine learning algorithms to optimize its predictive accuracy through the analysis of large datasets of patients who have already undergone knee joint replacements.
More broadly, Yushy’s research interests focus on hip and knee arthroplasty with the use of digital technologies to enhance patient outcomes and experiences. He has a medical degree from The University of Auckland and prior to his PhD has worked as an Orthopaedic Registrar in New Zealand.
Awards/Scholarships
Research Training Programme Scholarship, The University of Melbourne, 2021
Professor Phillip Walker Scholarship, Vascular Foundation, 2018
Phyllis Paykel Memorial Scholarship, The University of Auckland, 2015 & 2018
Summer Research Scholarship, The University of Auckland, 2014
Casement Aiken Bursary, The University of Auckland, 2014
NZQA Scholarship, St. Bernard’s College, 2012
Recent Publications
Gupta VK, Zhou Y, Manson JF, Watt JP. Radiographic spine adipose index an independent risk factor for deep surgical site infection after posterior instrumented lumbar fusion. Spine J [Internet]. 2021 Apr 20; Available from: http://dx.doi.org/10.1016/j.spinee.2021.04.005
Zhou Y, Isaacs SJ. Novel methods to monitor and support the cutaneous microcirculation in burn wounds: A review. South African Journal of Plastic & Reconstructive Aesthetic Surgery & Burns [Internet]. 2019 Jun 5 [cited 2021 Jul 26];2(1):26–31. Available from: http://www.sajprasb.org.za/index.php/SAJPRASB/article/view/1395
Research Assistant
Research Assistant
Amanuiel Taddese
OUR PEOPLE

Email: rita.kinsella@svha.org.au
- Gluteal tendinopathy
- Osteoarthritis
- Shoulder Injuries
- Department of Surgery, University of Melbourne
Rita Kinsella
BSc (Hons) Physiotherapy; M App Sci (Research)
Rita is an Advanced Musculoskeletal Physiotherapist and Clinical Researcher at St Vincent’s Hospital Melbourne. She completed her Masters (Research) on the evidence-based management of subacromial pain syndrome through La Trobe Sports and Exercise Medicine Research Centre, in 2018. She is now enrolled in her PhD, at the University of Melbourne, Department of Surgery at St Vincent’s Hospital, evaluating the prevalence and impact of gluteal tendinopathy in people undergoing total hip arthroplasty. As an early career researcher, Rita has led and worked on a variety of research projects involving interventions for musculoskeletal conditions including hip and knee osteoarthritis and shoulder pain, as well as studies informing the implementation of advanced musculoskeletal physiotherapy services within public health settings.
Awards/Scholarships
PhD RTS Scholarship, University of Melbourne, 2021
Kinsella R, Dowsey M, Page C, Pizzari T, Heywood S, Ma F, Choong P, Semciw A. Prevalence and impact of gluteal tendinopathy in people undergoing total hip arthroplasty. St Vincent’s Hospital Research Endowment Fund, 2019.
Kinsella R, Pizzari T, Cowan S. Isometric Exercise for rehabilitation of rotator cuff tendinopathy. Arthritis Australia Zimmer Biomet Award, 2017.
Research Assistant
Research Assistant
Amanuiel Taddese
OUR PEOPLE

Email: bccon@student.unimelb.edu.au
- Indigenous health
- Arthritis
- Physiotherapy
- University of Melbourne
Brooke Conley
Bachelor in Exercise Science and a Master of Physiotherapy Practice
Brooke Conley is a proud Ngiyampaa woman from Cobar, New South Wales. She has completed her Bachelor in Exercise Science and a Master of Physiotherapy Practice at Latrobe University in Bendigo. Brooke is a current PhD candidate at the University of Melbourne within the Department of Surgery. Her research will focus on developing culturally appropriate information and education resources for Aboriginal and Torres Strait Islander Australians with Osteoarthritis, Rheumatoid Arthritis, Lupus and/or Gout.
She’s passionate about improving health outcomes of Indigenous Australians and focuses on this in her positions as a First Nations health tutor at University of Melbourne and as a committee member for the Australian Physiotherapy Association (APA) Aboriginal and Torres Strait Islander health committee. Additionally, Brooke practices as a Physiotherapist at City Baths Spinal and Sports Medicine Clinic in Melbourne.
Contact
Research Assistant
Research Assistant
Amanuiel Taddese
OUR PEOPLE

Email: l.hawke@latrobe.edu.au
- Osteoarthritis
- Total knee and hip joint replacement
- Physical activity
- La Trobe University
- Eastern Health, Box Hill, Australia
Lyndon Hawke
BPhysio; MClinRehabNeuroPhysio
Lyndon Hawke has a background as a rehabilitation physiotherapist and is currently involved in stream 4 of the OPUS CRE that has a focus on redesigning a recovery program for TJR. Lyndon is currently investigating the reasons for, and possible ways to overcome, low physical activity levels after total joint replacement. Low physical activity levels in this patient population are a problem as people who have low physical activity levels have an increased risk of other serious health conditions e.g. cardiovascular disease.
Apart from his involvement in the OPUS CRE, Lyndon is taking part in the MIHip research trial as a motivational interviewer, and has clinical interests in community rehabilitation and vestibular
rehabilitation.
Research Publication:
Hawke, L. J., Shields, N., Dowsey, M. M., Choong, P. F., & Taylor, N. F. (2019). Physical activity levels after hip and knee joint replacement surgery: an observational study. Clinical rheumatology, 38(3), 665-674.
Hawke, L. J., Shields, N., Dowsey, M. M., Choong, P. F., & Taylor, N. F. (2020). Effectiveness of behavioural interventions on physical activity levels after hip or knee joint replacement: a systematic review. Disability and rehabilitation, 42(25), 3573-3580.
Scholarships:
Lyndon Hawke is the recipient of a Scholarship awarded through the NHMRC Centre for Research Excellence in Total Joint Replacement (APP1116235).
Research Assistant
Research Assistant
Amanuiel Taddese
OUR PEOPLE

Email: amanuiel.taddese@unimelb.edu.au
- Obesity, T2D and NAFLD
- Public and Global Health
AManuiel Taddese
BSc (Hons)
Amanuiel is a Research Administrative Assistant with OPUS, working behind the scenes to support the centre. He completed a Bachelor of Science with Honours at the University of Melbourne, and spent his research year investigating the role of liver-secreted proteins in exacerbating non-alcoholic fatty liver disease (NAFLD). He is also passionate about public health and reducing health inequities.
In his role, Amanuiel completes a number of administrative tasks including creating content and running our social media accounts. He also provides research assistance to a number of studies across a number of streams.
Awards
2019 RD Wright Prize
Consumer and Community Involvement Update
Amanuiel Taddese
NEWS
Consumer and Community Involvement update
By Amanuiel Taddese
What's Going on with the CCIP?
Our CCIP has started the year off with a bang, recruiting more community members and growing its reputation. The CCIP is now up to 10 members – reaching the target number for our pilot program- and are still recruiting participants! New consumers will shortly commence orientation and training, bringing them up to scratch on our work at OPUS and how they will be able to get involved. Following this, consumers will be matched up with researchers and formally begin the program in a capacity specific to the tier of involvement.
Likewise, as the program forges ahead, the team is now actively looking to recruit more researchers to partner up with our consumers. Researchers will be provided with the opportunity to engage consumers in their research by having a working partnership with a community member. A critical step for any research that desires to develop and deliver effective, personalised care.
One partnership that has already begun to work together is that of our PhD candidate Daniel Gould and our very first consumer advocate, Marion Glanville Hearst. The pair are research buddies and recently along with Consumer and Community Officer, Dr Tilini Gunatillake, were invited to speak at the Spotlight on Engagement webinar series hosted by the Melbourne Centre for the Study of Higher Education.
They did both OPUS and the CCIP proud, discussing the origins of the CCIP, the intricacies of the program and the experiences of both Daniel and Marion as research buddies. The talk garnered a great deal of interest and received great feedback from all in attendance.
Well done team!
Watch Tilini, Dan and Marion’s webinar below.
Amanuiel Taddese
OUR PEOPLE

Email: ryan.prehn@unimelb.edu.au
- Aboriginal and Torres Strait Islander Health
- Osteoarthritis in Aboriginal communities
Ryan prehn
BA
Ryan is a Research Assistant with the ECCO program (Enhancing Equity, Collaboration and Culturally Secure Osteoarthritis Care for Aboriginal Australians). He is currently completing the Bachelor of Arts at the University of Melbourne, majoring in Australian Indigenous Studies and Sociology.
In his role, Ryan engages in community liaising, relationship building, participant recruitment, data collection and analysis and advises on cultural security.
Awards
Murrup Barak Melbourne Institute for Indigenous Development Studentship
Miltiades and Alkistis Chryssavgis Scholarship
Wilson Dilworth Foundation Bursary
Amanuiel Taddese
NEWS
QUalitative research course
By Samantha Bunzli
What is OPUS' Qualitative research course?
Einstein once said: “Not everything that can be counted counts and not everything that counts can be counted.”
If there is a phenomenon in your clinical practice or clinical research that interests you and can’t have a number assigned to it, then our course is for you!
Qualitative research applies robust methods to study the ‘uncountable’ such as the patient experience of health and healthcare or how clinicians apply evidence in practice. By understanding these ‘social’ phenomena, we have an opportunity to advance clinical research and practice through the design and implementation of the right care, delivered to the right person at the right time.
Run over two half days, in this online course you will i) gain an understanding of qualitative research theory, methodology and ethics ii) develop skills in formulating a research question; recruiting and interviewing participants; analysing data and presenting findings.
You will have the option to attend an additional half day to workshop your own qualitative research project and receive mentor and peer feedback.
Dates have been locked in:
Section 1: 28th and 29th April 12-5pm
Section 2: 23rd June 12-5pm
Veronique Price
OUR PEOPLE

- Osteoarthritis
- Periprosthetic joint infection (PJI)
Elise Naufal
BArts (Criminology) (Hon), PhD (enrolled)
Elise Naufal will be commencing her PhD with the University Melbourne’s Department of Surgery in 2021. She has previously completed a Bachelor of Arts (Honours) in Criminology and will be transferring into the PhD from a Masters of Epidemiology. Over the last year, she has worked with the OPUS team as a research assistant for several projects.
Elise’s PhD project will draw on data from a recently established international periprosthetic joint infection (PJI) registry, which aims to provide insight into how treatment outcomes can be improved for patients who experience this devastating complication. Her project aims to identify patient and treatment related factors that predict successful management of these infections.
Scholarships
R.G. Wilson Scholarship (Honours)
Consumer & Community Involvement at OPUS
Veronique Price
NEWS
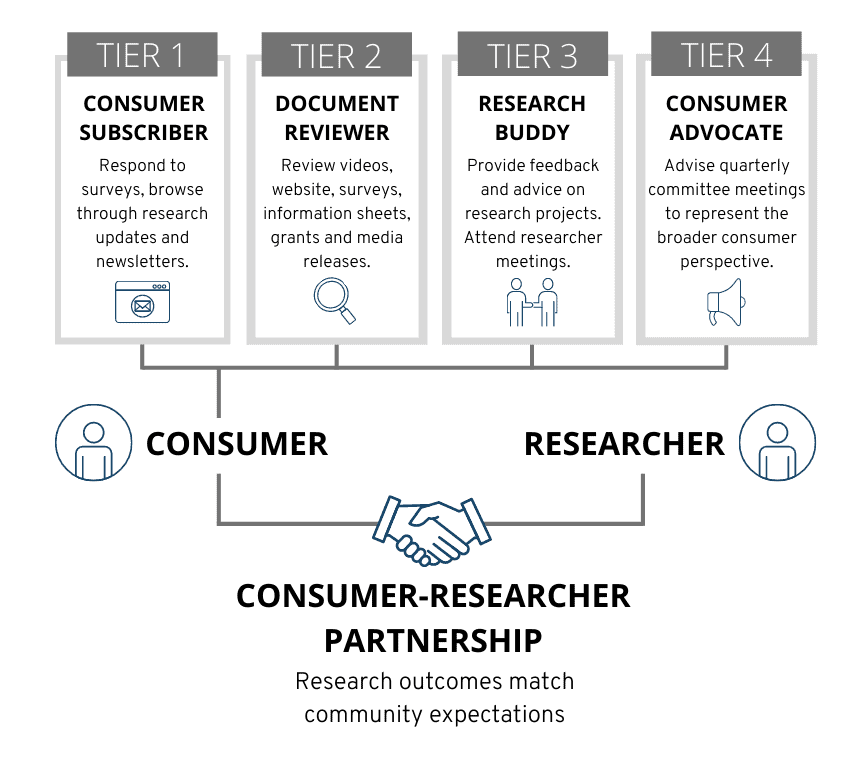
The Consumer and Community Involvement Program (CCIP) offers consumers the opportunity to participate in research programs. It’s about partnering with researchers to improve health care.
In turn, researchers receive an invaluable fresh perspective on the appropriateness, relevance and applicability of their research program. By engaging consumers throughout the research project cycle, we ensure our research outcomes meet community expectations.
OPUS welcomes interested members of the public with little-to-no scientific background, of any age or gender, to participate in osteoarthritis-related research projects.
CCIP: A year in review
Consumer involvement has always been a highly desirable complementary program to research groups. A small working group within OPUS was established to create this program a working reality and by March 2020, OPUS had assigned a Consumer and Community Liaison Officer to drive our concepts to implementation. Our framework has now been published as a protocol in Research Involvement and Engagement, which outlines how to embed consumer and community involvement within an established research centre. It details an actionable framework that moved beyond the current NHMRC general recommendations, so that other research centres can adapt the approach and learnings of the OPUS CCIP to their own research practices. The protocol also garnered significant interest online and across social media platforms, being picked up by Twitter users from Australia, France, Canada, Serbia and Pakistan.
Advertisement through word of mouth, social media, St Vincent’s Hospital outpatient clinics and the MSK newsletter has enabled us to welcome a total of nine consumers to the program, with more expected to join in 2021.
What to expect for 2021
Our CCI Pilot Program is set to commence in early 2021, starting with orientation and training for our newest members. These will bring consumers up to scratch with our work here at OPUS, share the opportunities available for them and provide a platform for networking between consumers and researchers alike.
Following orientation and training, consumers in the program will be matched with researchers dependent on their level of involvement within the four Tiers.
We have several other exciting consumer engagement events on the horizon for 2021, including a webinar with the Melbourne Centre for the Study of Higher Education as a part of the ‘Spotlight on Engagement’ series. We also have plans to host a ‘Consumers and Researchers: In Conversation’ event and an entire segment of the 2021 OPUS Forum will be dedicated to showcasing the CCIP.
After a year of meticulous planning and dedicated work, the CCIP is officially coming to the fore.
We are incredibly excited for the year ahead and we hope you are too!
Get in touch with our Consumer and Community Liaison Officer Dr Tilini Gunatillake if you have any questions about the program or fill out an expression of interest if you or someone you know would like to join the program.
Click the button below and scroll down to the ‘Expression of Interest’ form.
Consumer Spotlight: Marion Glanville-Hearst
Veronique Price
NEWS
We sat down to chat to Marion, our first consumer advocate here at OPUS.
Marion has not only provided invaluable insight in our recent publication on consumer involvement and partnered with PhD student Daniel Gould, but has also played a major role in shaping the OPUS consumer and community involvement program itself.
As you may have read in our article, consumer involvement is incredibly important in research. We are all working to improve health care for patients and community members affected by osteoarthritis, so why don’t we engage with them regularly and within a structured framework?
The first in a new series, here is the story of Marion Glanville-Hearst:

Marion is a retired occupational therapist, having spent much of her career working in psychiatry. Life circumstances took her the US where she studied a Bachelor of Psychology and Masters of Medical Anthropology, however as she was unable to find work in this area upon her return to Australia, she continued to work as an occupational therapist at St Vincent’s and many other hospitals in Melbourne. Marion also taught childbirth relaxation classes to expecting parents.
In 1994, Marion found out she had osteoarthritis developing in her hip and though the standard treatment was a total hip replacement, her GP advised her to put off surgery as long as possible as the prostheses ‘don’t last forever’ and replacing the glued-in parts would cause considerable damage for someone her age. With her background in healthcare and the savviness of her concerned son, Marion and her son began to read widely on total hip replacement surgery and osteoarthritis. She was shocked to discover the then-standard practice of metal-on-metal joint replacements were found to be correlated with metallosis: the build-up of metal debris in soft-tissues of the body. She continued to read the literature available and was also referred to a rheumatologist for assessment and to discuss non-surgical treatment alternatives. She continued to look after herself and had regular appointments with a myotherapist to help her mobility. In 2013, after 19 years of staving off the suggestions from exasperated friends and colleagues to ‘just get the surgery’, Marion elected to undergo a total hip replacement at a time she felt was right for her. From being so stiff that she could barely walk around her home, she regained the mobility and freedom she had 20 years prior. Her surgery was a success.
In the lead up to her surgery, Marion was alerted to a study being run by St Vincent’s Hospital Department of Orthopaedics through the osteoarthritis outpatient clinic she attended. The study, run by Prof Peter Choong and Dr Liz Nelson, was investigating if completing a MBSR (mindfulness based stress reduction) program prior to joint replacement surgery resulted in improved outcomes after surgery. After the study’s completion, Marion reached out to Liz, curious about the study’s results and the project’s research process. OPUS chief investigator A/Prof Michelle Dowsey then contacted Marion and proposed a novel idea for the research centre: a consumer and community involvement program. Marion joined the Steering Committee for the Consumer Engagement Working Group in late 2019 and has been involved ever since. She has played a pivotal role in shaping the program and building it from the ground-up.
Marion is formally a Research Buddy in Tier 3 of the CCIP framework. She has played a key role in the OPUS working group who have been working behind the scenes in 2020 to develop the CCIP framework and works closely with Dr Tilini Gunatillake, OPUS’ Consumer and Community Liaison Officer to continually improve the program’s processes. She also provides feedback on Daniel Gould’s PhD project: the development of a machine learning-enabled risk prediction tool for total knee replacement recipients and the investigation of the views of patients and surgeons on the use of artificial intelligence in healthcare.
For Marion, “being a member of OPUS and being able to include the perspective of a consumer in research programs has been very satisfying, as has been working with clinicians and researchers who want to improve outcomes for people like me.”
For more information about the OPUS Consumer and Community Involvement Program, please click here.
Veronique Price
NEWS
OPUS Spotlight: Elise Naufal