Difficulties in determining the impact of a risk factor that is handled in almost as many ways as the number of studies that report it
Article by Daniel Gould, University of Melbourne MD-PhD student
Osteoarthritis is a debilitating condition as well as a growing global health problem and total knee arthroplasty (TKA) is an effective treatment for advanced disease. Unplanned 30-day hospital readmission indicates post-operative complications, which disrupt the patient’s recovery journey and impose a significant financial burden on healthcare systems. Daniel Gould and his team reviewed the literature to better understand the patient-related factors associated with unplanned 30-day readmission following TKA.
Unsurprisingly, sicker patients are at higher risk of being readmitted compared to more healthy patients. Bleeding disorder, diabetes, chronic kidney disease and dialysis, chronic immunosuppressant use, and history of cancer each strongly increased a patient’s risk of readmission. Other conditions that increased a patient’s risk of readmission included dementia, depression, heart disease, respiratory disease, liver disease, and stroke.
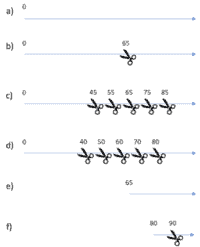
The evidence was not clear for the impact of sex, age, and body mass index (BMI) on readmission risk. Age and BMI are both positive ‘continuous’ variables, simply meaning they are measurements that take on any value greater than zero, up to a reasonable biological limit. However, researchers commonly categorise these variables. This means they select cut-points at which they split patients into various groups. Figure 1 shows illustrates some of the ways this can be done for age, and Figure 2 for BMI. Whether or not categorisation should be done at all is hotly debated amongst statisticians, and it was well beyond the scope of this review to settle the debate. The implication is that it is very difficult to compare findings between studies that chop up age and BMI in different ways. For example, it is difficult to determine the impact of age on readmission risk when comparing a study that uses method b) in Figure 1 with studies that use a different method.
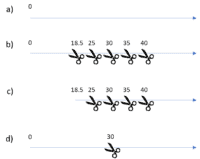
The purists would maintain that categorising continuous variables is never a good idea and argue that a) is always the correct way to handle continuous variables. However, the reality is that categorisation is a common practice and is further complicated by the fact that there is a widely accepted and well-documented way of categorising BMI laid out by the World Health Organisation (WHO) – Figure 2 b)– but there is no such system for age and as such researchers develop their own systems.
This narrative review highlights some of the difficulties in determining readmission risk based on common patient-related risk factors and also highlights the need for a systematic review and meta-analysis. This would provide one paper that comprehensively summarises the evidence from all the scientific papers published on this topic, which is more than 60 individual papers. The point is that orthopaedic surgeons use this literature to better inform the process of consent and shared decision-making for patients who are candidates for total knee replacement. It is also important that common patient-related factors are comparable because they can inform the development of a tool that automatically predicts a patient’s readmission risk based on their unique characteristics. To categorise or not to categorise: it seems like a niche statistical problem, but it can have wide-spread effects. Policy and decision making, and ultimately, patient health outcomes, depend on mitigating these inconsistencies.
To read Daniel’s narrative review, please click here.